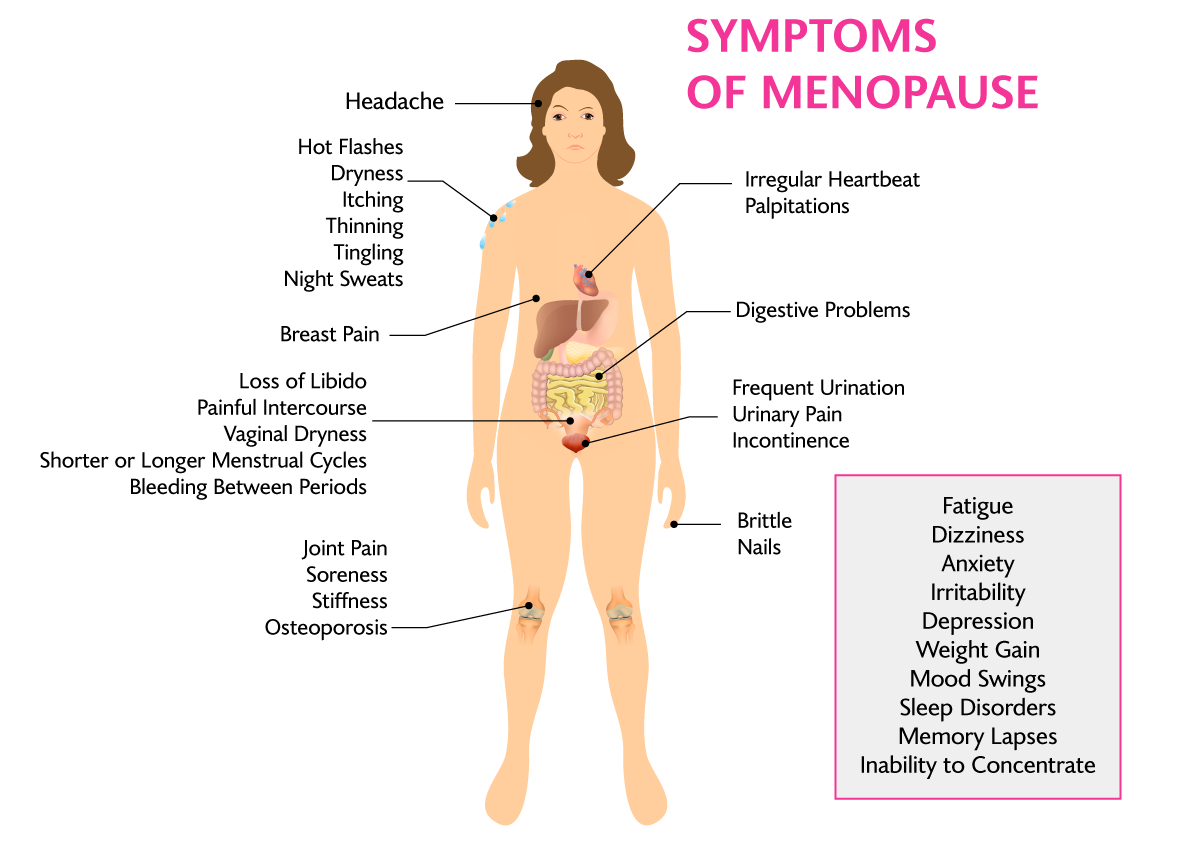
Common Symptoms of Menopause
Hot Flashes and Night Sweats
Hot flashes and night sweats, clinically known as vasomotor symptoms, are the most commonly reported symptoms of the menopause transition. One large, diverse US study found that up to 80% of women experience these symptoms at some point during the menopause transition.
Hot flashes are characterized by a sudden, intense sensation of heat in the upper body—particularly the face, neck, and chest. Each hot flash episode typically lasts between 1 and 5 minutes and may be accompanied by sweating, chills, and anxiety. Some women can feel a rapid heartbeat at the same time. Night sweats are hot flashes that occur during sleep. Chills can also occur, resulting in shivering. These are all disturbances in thermoregulation or regulation of temperature control. Some women experience hot flashes for a few years, whereas others may have them for decades.
We provide extensive counseling around non-hormonal and hormonal treatments, as well as lifestyle modifications to help you live your best life moving forward.
Genitourinary Symptoms
Genitourinary symptoms are a collection of signs and symptoms associated with estrogen deficiency that can involve changes to the labia, vagina, clitoris, bladder, and urethra. Genitourinary symptoms may be more severe in women who undergo menopause as a result of surgical menopause or because of chemotherapy for cancer treatment. They also may be more severe for women who take aromatase inhibitors for prevention or treatment of breast cancer.
Unlike vasomotor symptoms, which generally improve over time, these symptoms often worsen over time without treatment. Fortunately, there are many effective treatment options, including over-the-counter and prescription therapies.
Common symptoms include:
- Genital symptoms: chronic dryness, irritation, and burning. Many women feel as if they are getting recurrent yeast infections.
- Sexual symptoms: pain with vaginal penetration, decreased libido
- The dryness and thinning of the vagina that follows the drop in estrogen around menopause is the most common cause of painful sex at midlife and beyond.
- Less estrogen means less vaginal lubrication and a less stretchable vagina. The vagina also may shorten and become tighter at the opening. In some women, this can lead to a feeling of vaginal tightness during sex along with pain, burning, or soreness. Inflammation and irritation also can develop, leading to greater discomfort and sometimes to the tearing and bleeding of tissue with any penetration of the vagina. The pain can intensify to a point where sexual activity is no longer pleasurable or desirable, or it may not even be possible.
- Urinary symptoms: incontinence, recurrent urinary tract infections
- Estrogen helps protect the health of the bladder and urethra. With menopause, numerous urinary symptoms may develop, including a sensation of burning or pain with urination, increased frequency or urgency of urination, and increased risk of urinary tract infections.
- Women may feel urinary urgency with or without episodes of urine leakage (urinary incontinence) with increased daytime urinary frequency. Along with this, women may awaken two or more times in the night to urinate—a symptom known as nocturia.
Mood Changes
Estrogen receptors are widely distributed in the brain, including in the regions involved in mood regulation. Mood symptoms may be related to big swings in estrogen levels during perimenopause, but the precise mechanism isn’t known. Some women also experience changes in lifestyle behaviors (such as exercise levels or eating habits), sexuality, and other aspects of their health that have an effect on mood. The presence of stressful life circumstances or events may play a role, as can the presence and severity of menopause symptoms such as hot flashes and sleep changes.
Abnormal Uterine Bleeding
What is considered a normal menstrual cycle varies greatly from woman to woman. Still, in the years approaching perimenopause, most women will have a pattern that’s fairly consistent, so any changes in their bleeding pattern may be noticeable. It can be useful to track the bleeding on a calendar or app so that it can be easily reviewed and assessed.
Abnormal bleeding is not always a function of normal menopause. Most of the time it is, but abnormal bleeding can also be a sign of another health condition or even cancer. In cases such as cancer, the earlier that symptoms can be identified and diagnosed, the greater likelihood of successful treatment. Other possible causes of abnormal bleeding include fibroids, infections, thyroid dysfunction, and the use of certain medications or herbal products. Heavy or irregular bleeding, even when not related to cancer, can have a negative effect on quality of life.
Cardiovascular Disease
The American College of Cardiology/American Heart Association (ACC/AHA) Guidelines recognize the postmenopausal state as a risk factor for Cardiovascular Disease. The increased risk may be due to a change in the lipid profile such as an increase in low density lipids (LDLs).
Body Composition
During the postmenopausal period women often gain fat mass, central abdominal fats, and lose lean mass. This may lead to a spontaneous decrease of activities, decrease in energy expenditure, and decreased metabolic rate.